Every 20 seconds, somewhere in the world, a lower limb is lost due to diabetes. In Fiji a diabetes related amputation is carried out every 12 hours.
The World Health Organisation (WHO) estimates that 50% of all hospital admissions and amputations as a result of diabetes can be prevented with appropriate foot care. This has been supported [pdf] by the 40-60 per cent decrease in amputation rates during the last 10-15 years in countries with strong diabetic foot management services such as the United Kingdom, Denmark, Sweden, Australia and the United States. Unfortunately the same reductions are not being seen in low to middle income countries, where, in most cases, amputation rates are steadily increasing.
In 2014 Polynesia and Micronesia had the world’s highest age-standardised diabetes prevalence rate — nearly 25% — with Melanesia not far behind. With high rates of diabetes also comes a high prevalence of diabetic foot complications and resultant hospitalisations and amputations. This is evident with any visit to a Pacific Island hospital, where in many cases entire wards are full of clients with diabetic foot sepsis.
In June 2015, Motivation Australia, in partnership with the Samoa National Health Service (NHS), established a Diabetic Foot Clinic (DFC) at the Tupua Tamasese Meaole (TTM) hospital in Apia as part of the DFAT funded Samoa Integrated Mobility Device Service project. As discussed in a previous blog post, the multi-disciplinary DFC was introduced in order to reduce amputations and improve outcomes for clients with diabetic foot ulcers. The NHS DFC was established with a core team comprising of a podiatrist, nurse and orthotist, with support from doctors from the medical ward. Previous to the Diabetic Foot Clinic initiative there was no structured outpatient service for the prevention and treatment of these wounds and in many cases no treatment was sought until life-threatening infections occurred. As people present so late to hospital (for a variety of reasons), hospital admission to treat the sepsis often led to lower limb amputation (105 cases in 2014).
A previous evaluation of the NHS DFC showed good clinical outcomes for clients, however it did not objectively demonstrate the cost-effectiveness of the service to governments and donors — an essential element if the service is to expand in Samoa or other countries around the Pacific. To address this, a retrospective study comparing the costs and benefits of the NHS DFC, with treatment options available to clients prior to its implementation was undertaken. In Samoa the only recognised and measurable intervention for clients with diabetic foot ulcers prior to the DFC was inpatient treatment. As a result the costs and benefits of the DFC were compared to acute hospital care and amputation within TTM Hospital. The study was conducted as part of a partnership between the University of Twente, Motivation Australia and the NHS.
Medical records were reviewed for clients who were admitted at TTM Hospital for a diabetic foot ulcer for a two-year period between June 2013 and June 2015, and for clients who were treated for a diabetic foot ulcer at the DFC for the period June 2015 until May 2016. Costs of treatment were established for hospital inpatients and clients of the DFC.
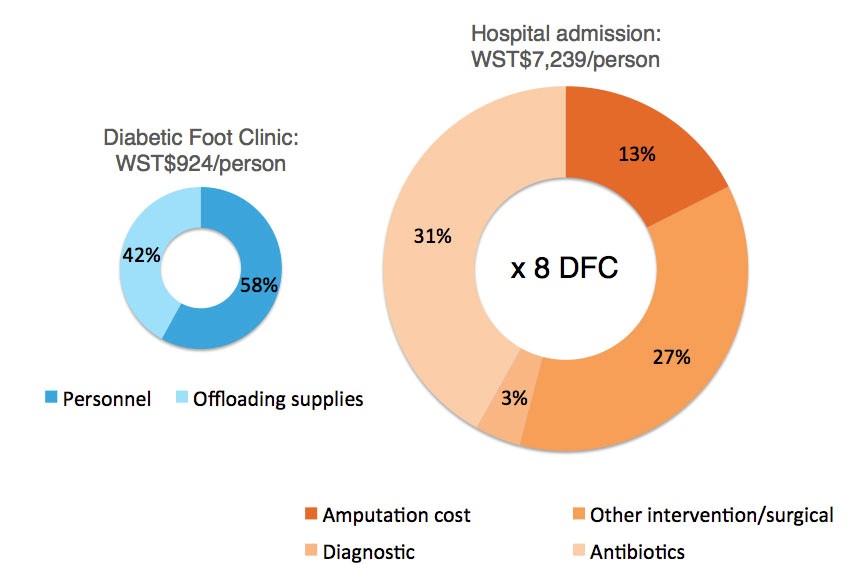
DFC costs were calculated using the mean costs of offloading materials per client who received offloading (removing pressure from an ulcer and redistributing it to other parts of the foot), and the mean salary costs per visit multiplied by the average number of appointments. Treatment costs in the TTM Hospital had to be calculated differently as there was no information available about the surgery costs, antibiotic costs and diagnostic costs. Hospital costs were therefore calculated using the Eurodiale study as a guideline. A percentage of amputation costs, intervention costs, diagnostic intervention costs and the costs of antibiotics were calculated from the total hospital costs. The hospital stay per day per bed at the TTM Hospital was 446 Tala, including administrative expenses and personnel costs. These costs were used to estimate the total direct costs per client.
Figure 1: Treatment costs for clients with diabetic foot ulcers seen at the DFC compared to those admitted to TTM Hospital
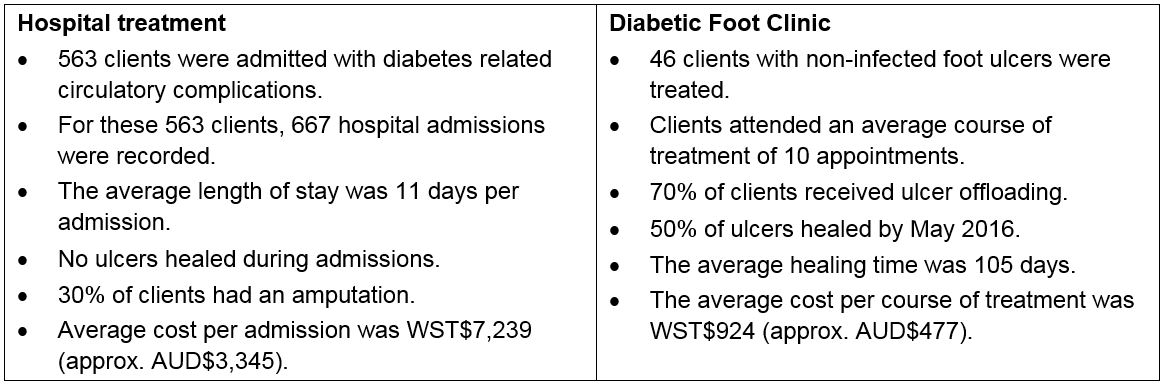
A summary of the findings of the research can be seen in the table below:
The treatment costs of the DFC are nearly 8 times lower when compared to the costs of admitting a client with diabetic foot sepsis into TTM Hospital.
Along with the economic benefits of the DFC over hospital admissions, outcomes for clients are also much improved. DFC clients were more likely to heal their ulcers, prevent infection and avoid amputations. The diabetic foot ulcers of clients admitted to the TTM Hospital, when compared to those seen at the DFC tended to have the added complication of infection. Within this study an assumption was made that treatment at the DFC prevented infection and the need for hospitalisation, and therefore the associated costs. This is supported by the fact that only one of the 46 clients receiving treatment at the DFC required admission to TTM with foot sepsis in the one-year period. The study indicates that the DFC could save costs for the NHS while improving outcomes for clients. Savings would increase and more people would benefit if the capacity of the service was expanded and Samoans were encouraged to seek treatment earlier at services closer to their communities.
The results show that the implementation of a dedicated Diabetic Foot Clinic both reduces costs and improves outcomes when compared to acute care, hospital admission and amputation. It is hoped that these findings can be used to encourage the establishment of more multi-disciplinary Diabetic Foot Care services within Samoa and throughout the Pacific.
Katrina McGrath is a Prosthetist Orthotist working as a Clinical Project Officer for Motivation Australia, a not for profit disability and development organisation, working in partnership with local organisations to enhance the quality of life of people with mobility disabilities in the Asia Pacific Region.
Thank you to Marjolein Wiegman of the University of Twente and the personnel and clients of the NHS, particularly the Diabetic Foot Clinic, for their assistance.


It is good to see some actual numbers being used to assess this situation. It is also interesting, and important, to see that the Diabetic Foot Clinic was able to achieve both improved clinical outcomes (reduced infections etc) as well as significantly reduced financial costs compared to the hospital based care, thereby potentially freeing up health resources that can be reallocated to higher impact interventions.