When Billy Graham talked to a third of a million Africans in 1960, ‘an overwhelming majority of them black, and saw some 20,000 of them raise their hands as a sign they were ready to receive Christ as saviour,’ his success demonstrated that mass evangelism ‘may well be possible in Africa.’
Throughout his six-week, 14,000-mile crusade, Graham showed ‘evangelistic zeal to everyone he met.’ He emphasised that Jesus Christ had come from the crossroads of Asia, Africa and Europe and ‘had lived in Africa when his parents fled to Egypt and was aided by an African, Simon the Cyrenian, on his way to the cross.’
Graham also paid tribute to ‘the missionaries whose work paved the way for his own evangelism,’ but Life Magazine’s March 21, 1960 article doesn’t mention his praying for me.
In March 1960, Graham visited Bingham Memorial Hospital in Jos, Nigeria, to visit and pray for my father who had drug-resistant malaria and filariasis, and for my mother who was seven months pregnant with me.

From the late 1950s to the mid-1970s my parents worked for the Sudan Interior Mission (SIM), first in west Africa and later in Ethiopia. From the 1930s, SIM sought to bring evangelical Christianity into the ‘unoccupied regions’ (Rowland Victor Bingham, founder of the SIM, cited in Donald Donham’s book Marxist Modern: An Ethnographic History of the Ethiopian Revolution). According to Donham, the missionaries used aspects of modernity, particularly technology and medicine, to propagate their Christianity. Their ‘principal appeal to Ethiopians came to rest precisely on their ability to offer an entrance to modernity, as it was locally constructed. Imbued with a progressive sense of time and increasingly impatient with “tradition,” mission converts dreamed of a better day.’
When we moved to Ethiopia in 1966—the high altitude deemed much better for my father’s health than the tropical heat of west Africa—the language I learnt described the literal connections between how world events (the Cold War, famine, drought, tribulation, pestilence and other natural disasters) brought us closer to the end times; and how we needed to believe in the second coming of Christ and the establishment of the millennial period when Christ will reign on earth. This language of dispensational premillennialism, as Susan Harding argues, is ‘a wilfully “mad rhetoric,”’ and ‘speaking it (being spoken by it) is a political act, a constant dissent, disruption, and critique of modern thought, and specifically of modern historical discourses that constitute hegemonic knowledge about world events, past and present.’
It was also the language of my dormitory supervisors and teachers at the boarding school named after Bingham; this ‘mad rhetoric,’ set within a framework of polarities of ‘right and wrong, good and evil, light and darkness, mammon and God, flesh and spirit, demons and angels, world temptations and heavenly salvation’ (see ‘Sources of Christian Fundamentalism in the United States’ here). My six-year old self became terrified—too scared to leave my bed at night lest Satan, the demon serpent, attack me in the dark, I started having nightmares and regressed to bed-wetting.
But other memories quarantined the authoritarian boarding school—memories of holidays in Kefa Zone in the southwest. Unlike other landscapes in Ethiopia—highland plains, mid-land plateaus, valley bottoms and vast escarpments in the north—desert scrubland with shallow salty lakes and long chains of volcanoes in the northeast—all well known to outsiders for drought and famine, or as the ‘hottest place on earth,’ Kefa Zone is dominated by steep hills, gorges and streams. Compared to other parts of the country, there are still large areas with natural forest. These forests, renowned for their high biodiversity values, are also the habitat of wild Ethiopian coffee, the origin of the genetic diversity of Arabica coffee (Coffea arabica). Kefa Zone is like a collage affixed to the surface of waves of parallel mountains rolling away in the distance. A green collage. Juxtaposed on the closest wave—tall rainforest green; bamboo stalks deep, dull green; still green sorghum with ripening spikelets; stands of enset or false banana up to ten metres tall with dark green leaves four or five metres long and a metre wide; and small fields of tef grain grass almost yellow or a yellow almost green. Riding the waves in the distance, the green becomes dark purple, light purple, blue green, ultramarine blue. My childhood memories were of this Garden of Eden; a place I thought was paradise.

Almost 40 years later I returned to ‘darkest Africa’ while studying international development and wanting to understand why my parents worked there. I soon discovered that development has its own polarities: undeveloped and developed, traditional and modern, unsafe and safe, untrained and trained, illiterate and literate, race, religion and ethnicity, and so on.
And development expounds its own ‘mad rhetoric’ through economic development, basic needs, official development assistance, aid for trade, protection of basic services, universal health coverage and primary health care, the imperative for developing countries has been modernisation as development: reproductive health policies for instance, are based on modernisation by means of Western technology and its success with biomedicine. ‘Modernist conceptions of the future are dramatically different from evangelical ones,’ but there is also a sense that the shape of the modernist future ‘has to lead to gain and advancement… Because of the arrow of progress, particularly of technological progress, the future continually arrives ever more quickly. Time speeds up,’ Donham observes.
In 2007, I wanted to examine how reproductive health, in particular the goal of reducing maternal mortality, fitted into Ethiopia’s development agenda. Back in Kefa Zone, Bonga, the administrative centre was now a small town of around 20,000 people. Bonga had recently acquired (intermittent) 24-hour electricity, telephone, slow dial-up internet, and on the day of my arrival, limited mobile phone service. Besides talking to women about their experiences giving birth, and staff who worked at health centers or the hospital, I wanted to talk to the people who worked for NGOs and local government because they were the ones putting development policy into practice.

Almost all these people defined development as modernisation, using examples such as the construction of roads and bridges, clean water supplies, electricity and phones, the internet, schools, health posts, health centers, hospitals and so on—the more visible or tangible signs of change. Only two NGO staff argued that development could address other issues such as ‘freedom and security as well as the environment,’ or that development should consider minority groups who were excluded or given unequal access to transport, health services or education.
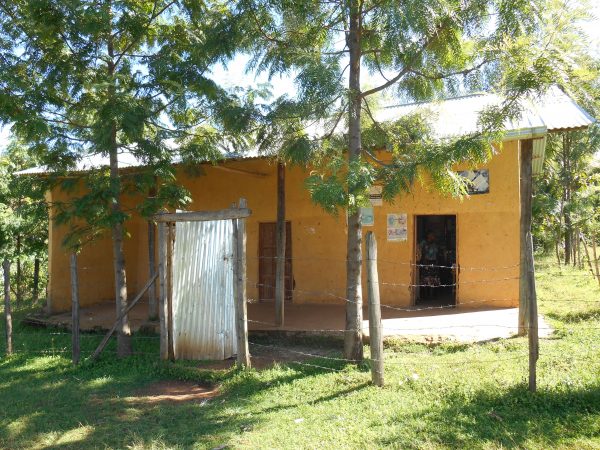
More recently, I worked as the Strategic Director at an NGO funded health centre in Kefa Zone. My main task was to draft the next five-year agreement between two NGOs and three levels of government. Although I wasn’t involved with day to day management, it was impossible not get involved when things happened concurrently: recently there was no electricity for three days; the generator broke down and still hasn’t been repaired; an administrative error meant we ran out of epilepsy medicine for the many epilepsy patients who come for free medicine every Thursday (it takes around a week to write the order and drive to the pharmacy warehouse 145 kilometres away, and then to record and put away all the medicines in the store room); and five nurses and midwives in the delivery room worked over their lunch break to stop a woman dying from post-partum haemorrhage. The next day the ambulance was called to pick up a woman who had retained placenta after giving birth at home. She had been staying in the maternity waiting home for a few days, but her husband insisted she go home to prepare for Ethiopian Christmas.

These experiences taught me that the problems of the Ethiopian health system are complex and cannot be reduced to simple fixes such as building health facilities if women cannot access them in time, if the care they receive is not respectful, or if the quality of care is insufficient, as in Genet’s case.
I met Genet in 2014. Genet is one of over 40,000 Health Extension Workers (HEWs) who are based in health posts in the villages or kebeles, with two HEWs assigned to each health post. They provide basic health services to each kebele of around 5,000 people. One of their roles is to assist women to prepare for birth and to mobilise communities to facilitate timely referral to mid-level or specialist care if needed.
Genet (a pseudonym) attended antenatal care at the hospital because she didn’t live too far away and hoped to get better service there during her first pregnancy. When Genet was around 39 weeks pregnant she went to the hospital, but the midwife told her to go home, saying that sometimes women can delay beyond the expected 40 weeks. Genet went to her parent’s home to wait. Three days later, at midnight, she thought she felt labour pains but was not quite sure. Two hours later the labour was quite strong and she called for the ambulance but was told it was being used elsewhere. Genet then phoned some friends to contract a taxi.
At 4 am, Genet arrived at the hospital accompanied by her parents, sisters and another HEW. After being admitted, the two midwives at the hospital told her that she still had some time and would not deliver until the morning: ‘Both midwives were listening to music through headphones on their mobile phones and did not bother to look after me,’ Genet explained.
By now Genet was crying and shouting because of the pain and one of the midwives slapped her and bit her, shouting, ‘Are you a Health Extension Worker? Shame on you. Just sleep and wait for the doctor to come in the morning.’
Genet slept a little and the midwives went to their room and slept.
At 8.30 am two different midwives came on duty and called the doctor at 9 am. The doctor performed a vacuum delivery.
‘After two hours, I heard my mother crying and realized that my child had died. I was told that during my stay in the hospital the child was deprived of oxygen,’ Genet said.
The amniotic fluid had affected the child through his nostrils and mouth during the delay in the hospital.
‘I was so frustrated with the death of my first child and felt the hospital service was hopeless, especially the care of the midwives. I wanted to complain to the hospital administration, but I feared their bureaucratic revenge on me and my job,’ Genet said.
When I met Genet she was apprehensive about getting pregnant again.
For Nigerian-American author Teju Cole, ‘Africa serves as a backdrop for white fantasies of conquest and heroism.’ I agree with Cole that much of what happens in many places in Africa is not as it should be. We have an ‘internal ethical urge’ to serve justice as much as we can. It’s true that one of the reasons I keep returning to Kefa Zone is to satisfy my own ‘emotional needs,’ but then again, it’s a very beautiful place to visit. Like Cole, I agree that a great deal has been done to improve health services in a place like Kefa Zone. And not only, or primarily, due to foreigners and NGOs. I think of the Ethiopians I know who choose to work in health centers in rural towns when they could earn a lot more if they moved to the city. And others who have worked for years on projects to reduce deforestation and protect the forest, in one of the world’s 34 biodiversity hotspots.
I don’t want to be a ‘white saviour,’ but if I’ve learnt anything so far, it’s that overcoming the difficulties women and their families face trying to access health facilities in rural Ethiopia should involve listening to the voices of the women themselves and not just listening to the ‘mad rhetoric’ of others.






How long before we are able to banish that dread disease: ‘white saviour syndrome’?
Great article. I like this personal historical approach.
It’s tough being poor and even harder being a poor woman.