This week, the world turns its attention to antimicrobial resistance (AMR) for WHO’s World Antibiotic Awareness Week (WAAW). WAAW campaigns for us all to ‘handle antibiotics with care’ and take urgent action to curb the spread of AMR, that could, without action, lead to an alarming 10 million deaths a year by 2050. With the recent launch of the Australian Government’s Health Security Initiative for the Indo-Pacific region, this is a timely reminder of the role the initiative must play in strengthening animal and health systems to address AMR.
At the forefront of this year’s WHO campaign is the critical role that infection, prevention and control (IPC) plays in preventing AMR in health care settings: “every infection prevented is an antibiotic treatment averted”. Health care facilities are high risk settings for the spread of infections and the development of drug resistance. If health facilities are unclean, do not have running water or soap for washing hands, do not have functioning toilets to contain human waste and do not have waste systems to safely dispose of health care waste, facilities can become epicentres for driving resistance. The very place that people go to seek care ends up making them, and the community, sicker.
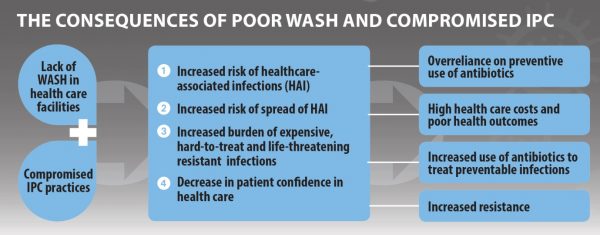
As outlined in the infographic below, poor water, sanitation and hygiene (WASH) and IPC in health care facilities increases the risk of healthcare associated infections, a problem which currently affects, on average, 1 in every 10 patients in developing countries. More seriously, many of these infections are antibiotic resistant, which can more than double the likelihood of death. Vulnerable groups accessing health services, such as women around the time of childbirth, newborns, and people living with HIV are more susceptible to such life threatening conditions, further increasing the risk of infections spreading.
When we look at the Asia Pacific region, previous efforts to address AMR have failed to address the basics in health care settings: water supply, adequate and safe sanitation, and good hygiene practices. This was most recently recognised in the evaluation of Australia’s response to combat pandemics and emerging infectious diseases, where special mention was made to how a lack of WASH in health care facilities compromised the ability to control infections and improve preparedness and resiliency against future outbreaks. Efforts to tackle emerging infection disease threats in countries across the region did not sufficiently address WASH, and coordination between WASH and health sectors was poor. This lack of coordination must be overcome if we are to address AMR and support health security more broadly in the region.
WHO/UNICEF global estimates suggest that almost 40% of health care facilities have no water supply, 20% do not have safe toilets and 35% do not have soap and water to perform basic hand hygiene. Knowing how important these basic services are to provide safe, quality health care, such alarming statistics reveal the extent to which global health security efforts are currently being compromised. There are currently no estimates of coverage of WASH in health care facilities for our region, with insufficient national level data to calculate regional estimates for the WHO Western Pacific Region (WPRO) and only a handful of national estimates to be drawn on for water and health care waste management (with insufficient data on sanitation) to generate regional estimates for the South East Asia Region (SEARO).
This lack of data is a problem that must be addressed. Without accurate data, realistic targets cannot be set and progress cannot be measured. In current health security efforts, it seems that “no data on WASH” is frequently interpreted as “WASH is not a problem”. We know that this is not the case. Small scale assessments underway in the region are showing that there are major WASH challenges that warrant immediate action.
There are three key WASH challenges to address which could help tackle AMR. Firstly, the lack of robust coverage data can, and should be, addressed. As part of WHO and UNICEF’s Global Action Plan for WASH in health care facilities, monitoring tools have been developed to track national and global progress on WASH in health care facilities. Basic indicators are available to monitor four core elements of WASH: water supply, sanitation, hand hygiene and health care waste management. Targets should be set to improve WASH across the region as part of AMR efforts and these indicators used to track progress.
Secondly, driving political will for action. WASH is repeatedly recognised as a fundamental cause and driver of AMR in health settings, yet when it comes to setting action plans and strategies, it is often overlooked. WASH in health care facilities should, and needs to be, prioritised in AMR strategies.
Finally, we must move beyond the misconception that ‘WASH = installing infrastructure’. Yes, the basic infrastructure is needed, but in time taps leak, toilets get blocked and water systems get contaminated. When we talk about WASH in health care facilities as a means to address AMR, we must also consider financing, human resources, training and sustainability. In tandem with this, we must also work to achieve long-term hygiene behaviour change. Health facilities are complex environments and focussing on infrastructure alone will not achieve a strong, resilient health system, capable of addressing and responding to the growing threat of AMR.
So, when we consider ‘handling antibiotics with care’ this week, we should also make sure we are only handling those antibiotics when absolutely necessary: not because of an infection that could have been prevented through improved WASH. Remember, “every infection prevented is an antibiotic treatment avoided”. Prevention is the first step to slowing AMR and improving health security, and WASH in health care facilities lies at the heart of prevention.
More information on how you can get involved in WAAW can be found here.
More information on WASH in health care facilities can be found here.



Leave a Comment