The latest World Obesity Atlas 2023 – yes, there is such a thing – has three important findings for countries globally, including those in the Asia-Pacific region. First, the prevalence of obesity is rising rapidly, especially in middle income countries and among the young. Second, obesity has very significant – but often avoidable – financial and economic impacts, as well as health impacts. Third, few low and middle income countries are adequately prepared to respond: for example, Papua New Guinea is ranked 182 out of 183 countries in the world in terms of “global preparedness”.
The Atlas reports significant increases in the prevalence of obesity at the global level. It notes, for example, that “every country is affected by obesity” (body mass index or BMI of ≥ 30 kg per metre of height squared) and that no country has reported “a decline in obesity prevalence across their entire population, and none are on track to meet the World Health Organization’s (WHO) target of ‘no increase on 2010 levels by 2025’”.
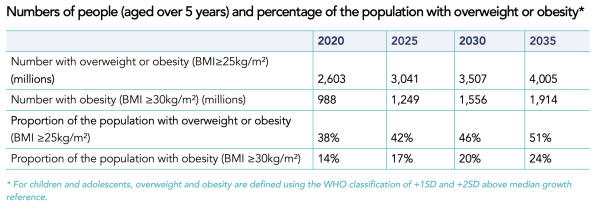
The report goes on to say that 51%, or more than 4 billion people, will be living with either overweight (BMI ≥ 25 kg/m2) or obesity by 2035 if current trends prevail; 1 in 4 people (nearly 2 billion) will have obesity. Figure 1 shows the projected increase in numbers, and increased proportion, of the population globally being overweight or obese between 2020 and 2035.
Figure 1: Global overweight and obesity, 2020-35
Source: World Obesity Atlas 2023, p. 11
The Atlas emphasises that the largest proportion of obesity globally already occurs in middle income countries. It estimates that, globally, just on 60% of men and women with obesity lived in middle income countries in 2020, with this share projected to rise to 70% by 2035. The share living in high income countries falls accordingly.
The Atlas also includes projections for the rise in obesity for different geographical regions. For example, it estimates the total number of adults living with obesity will more than double between 2020 and 2035 in both the WHO Western Pacific region – which includes China but also the Pacific Island countries – as well as the WHO South-East Asia region. Importantly, the prevalence of obesity (that is, the proportion of the population at a given point in time) is expected to double, on average, for key cohorts over that period as well (Figure 2). For example, the Atlas estimates the prevalence of obesity in men to increase from 8% of the adult population to 19% in the Western Pacific region, and for women to increase from 8% to 16% in the South-East Asia region, between 2020 and 2035.

One of the most interesting and useful, but potentially disturbing, parts of the Atlas is the assessment of individual countries’ “readiness to cope with the predicted rising levels of obesity, especially in its more severe forms, and the consequential NCDs [noncommunicable diseases] that arise”. In essence, the report draws on four sources of information to generate a “preparedness ranking” for 183 individual countries for which data is available.
The first source of data is the extent of effective universal health coverage in a country, using the 23 indicators that are tracked as part of the Sustainable Development Goals as at 2019 (latest year available). The second source of data is the WHO listing of premature deaths due to NCDs as a proportion of all NCD deaths, given the high degree of correlation between obesity and NCDs. The third source of data is the extent to which a country provides any of 13 NCD-related indicators in the public health system, for example, general availability of diabetes testing and/or total cholesterol measurement at the primary health care level, and general availability of statins in the public health sector. The fourth source involves data on 12 “NCD-related policy-related indicators for the prevention of NCDs at a national level”, including policies to reduce physical inactivity, salt consumption, unhealthy diets, and marketing of unhealthy foods to children.
Figure 3 summarises the preparedness rankings for countries in Asia and the Pacific. Switzerland (not shown) is ranked first out of 183 countries. Within the Asia-Pacific region the Republic of Korea is assessed as being the most prepared, ranked 17 out of 183 countries globally. Four countries in the region are in the top 34 countries of the world rated as “good” (dark green rows). The Atlas uses a traffic light classification with countries rated as “fairly good” (light green), through “average” (yellow), to “poor” (light red) and “very poor” (bright red). Eight countries in Asia and the Pacific are rated as “very poor”. Definitions of the terms used are on page 229 of the report.

There are some worrying scenarios for countries in the Asia-Pacific region. Of concern is that PNG is rated 182 out of 183 countries, that is, the second least-prepared country in the world after Niger, which is ranked last at 183. This is worrying because the Atlas estimates that the annual increase in adult and child obesity in PNG over the period 2020-2035 will be, respectively, 2.8% and 5.2% per annum. That, in turn, implies adults with obesity will be 38% of the population of PNG by 2035. The Atlas also has projections that by 2035 around two-thirds or more of the adult population will have obesity in a number of countries in the region including the Federated States of Micronesia, Kiribati, Samoa and Tonga.
On a more positive note, the Atlas rates Timor-Leste’s and Sri Lanka’s global preparedness as “fairly good” (ranked 44/183 and 40/183) with adult obesity prevalence of 12% and 14% by 2035 respectively. As lower middle income countries, Timor-Leste and Sri Lanka may therefore have program and policy lessons for other countries in the region. Identifying those specific lessons would be a useful subject for next year’s edition of the World Obesity Atlas.





Hi Ian.
A few points on this, as someone with lived experience.
This report in general is pretty light on, and doesn’t acknowledge the complexity of this issue, nor any insight into what works. And to me it is a huge, huge issue that the report is funded by pharma.
The World Obesity Foundation that publishes the Atlas is funded by a number of drug companies that are currently making very large profits from pushing the new generation weight loss medications such as semaglutide etc. Novo Nordisk for example, the manufacturer of Ozempic, which has had a worldwide shortage last year due to off-label usage as a weight loss drug, is listed as a key funder of the report!
It is worth noting that there is a huge financial incentive for these companies to continue to frame obesity as a curable condition stemming from individual choices or behaviours, rather than advocating for better health access for people with bodies of all sizes or examining the structural drivers, for example. There is also a financial incentive for these companies to see health systems frame obesity in this way instead of looking at more holistic or ‘health at any size’ approaches in their health systems.
Access to appropriate, quality, accessible, non-stigmatised medical care continues to be a huge issue for people with fat bodies in developed countries — is the same framing we have used in the West around this issue actually going to help in developing countries or just replicate the same issues? Thinking and language around this issue is evolving in Western medicine practice (albeit incredibly slowly) — this report makes a nod to some of this language to seem like they ‘get it’ in the priority section for example, but doesn’t really engage with it, particularly on what it might mean in a developing country health care setting.
Obesity as measured in the report is based on BMI solely, which is a measure with many known problems, particularly around race and ethnicity. The American Medical Association just last week adopted a new policy on the use of BMI, acknowledging its deep flaws. This report makes no acknowledgement of the limitations of the measure.
That’s just a few very quick things that concern me about the report that I just had to attach here. I think looking at NCDs themselves is much more useful — not all fat people have an NCD, not all people with NCDs are fat, etc. NCDs can be managed or prevented even if people remain in an overweight or obese weight category, etc.
Obviously we want to reduce incidence of NCDs and support people’s health (in a holistic sense, which I don’t think the BMI captures with accuracy or nuance).
But Novo Nordisk has some strong perspectives on the best way to do that and it involves a once a week injection into your upper thigh that currently retails for about $300 AUD a pen if you can even buy it.
(For those who want to learn more on some of these issues I highly recommend the Maintenance Phase podcast episodes, particularly the ones on BMI.)
Thanks Ashlee. Points noted!
The Report does largely focus attention on “what works” in terms of country level preparedness to respond to the rise of obesity and associated NCDs. For each country it first provides quite detailed and useful projections for the rise of obesity among male and female adults, and children, through to 2035 and, for those countries with sufficient data, estimates of the economic impact if existing trends continue.
As mentioned in the blog, the report then draws on four separate sources of (mainly WHO) data and a total of 48 separate indicators capturing aspects of “what works” in terms of access to health care, availability of services; and policies. The specific indicators are set out on pages 230 and 231 of the report.
Any country can therefore use all this to assess for itself how well it is providing known policies, services, and programs that “work”. The country rankings can also shed light on how well a particular country is implementing “what works” in relation to neighbouring and comparable countries. Identifying in even more detail the positive lessons from countries that do rate well in terms of their readiness and preparedness to respond to increases in obesity and NCD is recommended in the last paragraph of the blog for the future.
Thanks for your continued interest in these important development issues and contributing to the debate.
Ian